Definition
Chest physical therapy (CPT) is the term for a group of treatments designed to improve respiratory efficiency, promote expansion of the lungs, strengthen respiratory muscles, and eliminate secretions from the respiratory system.
Purpose
The purpose of chest physical therapy, also called chest physiotherapy, is to help patients breathe more freely and to get more oxygen into the body.
Chest physical therapy includes postural drainage, chest percussion, chest vibration, turning, breathing exercises, coughing, and incentive spirometry. CPT is usually done in conjunction with other treatments to rid the airways of secretions. These other treatments include suctioning, nebulizer treatments, and the administration of expectorant drugs.
Chest physical therapy can be used with newborns, infants, children, and adults. People who benefit from chest physical therapy exhibit a wide range of problems that make it difficult to clear secretions from their lungs.
Patients who may receive chest physical therapy include those with cystic fibrosis, neuromuscular diseases (such as Guillain-Barré syndrome), progressive muscle weakness (such as myasthenia gravis), or tetanus. People with lung diseases such as pneumonia, bronchitis, and some forms of chronic obstructive pulmonary disease (COPD), including chronic bronchitis, also benefit from chest physical therapy. CPT should not be used in the treatment of patients diagnosed with asthma.
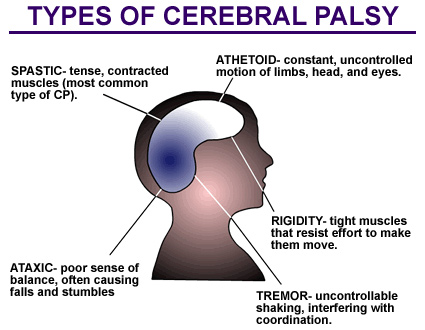
People without specific lung problems but who are likely to aspirate their mucous secretions because of diseases such as cerebral palsy or muscular dystrophy also receive chest physical therapy, as do those who are bedridden or confined to a wheelchair. In addition, CPT may be part of treatment after surgery for patients who develop difficulty taking deep breaths.
Precautions
While the doctor ultimately determines which type of therapy can be performed, health care professionals know that not all forms of chest physical therapy are appropriate for all patients. Postural drainage and percussion should not be administered to patients who:
- have just eaten or are vomiting
- have acute asthma or tuberculosis
- have brittle bones or broken ribs
- are bleeding from the lungs or are coughing up blood
- are experiencing intense pain
- have increased pressure in the skull
- have head or neck injuries
- have collapsed lungs or a damaged chest wall
- recently experienced a heart attack
- have a pulmonary embolism or lung abscess
- have an active hemorrhage
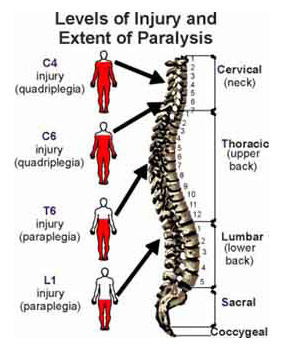
- have injuries to the spine
- have open wounds or burns
- have had recent surgery
Description
Chest physical therapy can be performed in a variety of settings including critical care units, hospitals, nursing homes, outpatient clinics, and in the patient’s home. Depending on the circumstances, chest physical therapy may be performed by anyone ranging from a respiratory care therapist to a trained member of the patient’s family. Patients can be taught to perform some therapies.
Lengths of therapies and their costs vary. Some therapies may be part of ongoing treatment for a chronic condition. Special equipment may be needed for some procedures, such as percussion, and may be covered by the patient’s health plan.
Chest physical therapy encompasses a variety of procedures; which ones are applied depends on the patient’s needs. Hospitalized patients are reevaluated frequently to establish which procedures are most effective and best tolerated. Patients receiving long term chest physical therapy are reevaluated about every three months.
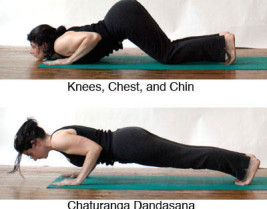
Turning
Turning from side to side permits lung expansion. Patients who cannot turn themselves are turned by a care- giver. The head of the bed is also elevated to promote drainage if the patient can tolerate this position. Critically ill patients and those dependent on mechanical respiration are turned once every one to two hours around the clock.
Coughing
Coughing helps break up secretions in the lungs so that the mucus can be suctioned out or expectorated. However, for patients with conditions like COPD, it can be painful to cough normally. An important part of chest
 A patient with cystic fibrosis receives chest physical therapy after using nebulizer therapy to loosen the mucus in her lungs.
A patient with cystic fibrosis receives chest physical therapy after using nebulizer therapy to loosen the mucus in her lungs.
physical therapy is teaching patients to clear their airways by gentler methods, such as with a controlled cough or by “huffing.”
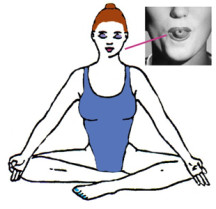
Before either technique, patients are advised to sit upright and drink a glass of water. For the controlled cough, patients purse their lips and take a deep breath. They hold their breath for several seconds and then make two brief, gentle coughs. Huffing also starts with pursing the lips and taking a deep breath. After holding the breath for several seconds, patients exhale by using the stomach muscles to push the air out. The vocal chords remain open so that the cough has almost a whispery sound. Coughing and huffing are repeated several times a day as needed.
Deep breathing exercises
Deep breathing helps expand the lungs and forces better distribution of the air into all areas. The patient may initially need to lie down to do these exercises, but eventually it is done while sitting upright, then while walking.
Patients may find it helpful to monitor their breathing by placing a hand on their abdomen to provide a sense of their regular breathing pattern. The patient then starts by taking a deep breath through the nose, then purses the lips as if to whistle. The patient then exhales the air slowly through pursed lips. The exhalation should take twice as long as the inhalation. A patient may start by inhaling for two seconds and then exhaling for four. After taking several deep breaths, the patient breathes at a normal rhythm and begins another cycle of deep breathing. The patient builds up to taking deeper breaths, following a schedule given by the health care team. Generally, COPD patients practice deep breathing exercises for 20 minutes each day.
Incentive spirometry
The incentive spirometer helps the patient improve lung function. This self-administered therapy involves inhaling into a tube attached to a device. The specific technique and goal depends on the type of spirometer. The patient receives directions from the doctor, nurse, or respiratory therapist.
With a breath flow-oriented device, the patient inhales through a tube to raise a ball inside the plastic spirometer chamber. The drop in pressure causes the ball to rise, and the goal is to keep the ball in the air for as long as possible.
For a volume-oriented device, the patient sets a pointer on the chamber at the desired breath volume level. The patient inhales into the tube and attempts to raise a piston inside the chamber so that the volume marker reaches that level.
Hybrid volume accumulators combine a flow-oriented device with a volume-oriented device. A piston inside a cylinder responds to negative pressure from the patient’s inhalation.
Some devices have a component designed for exhalation. If the model does not include an exhaling function, the patient breathes out air naturally.
At the end of the session, the patient takes a deep breath and then coughs. The length of therapy and the number of exercises done depend on the patient’s condition and is determined by a respiratory therapist or other health professional.
Postural drainage
Postural drainage uses gravity to assist in draining secretions from the lungs and into the central airway where they can either be coughed up or suctioned out. This therapy generally lasts a maximum of 30 minutes. If various positions are tried to induce a cough, the patient may remain in one position for from five to 15 minutes. The health care team guides the patient in determining the amount of time needed. Each position reaches a specific area of the lungs. Chest drainage positions include:
- the patient seated with head back
- the patient seated with head bent forward
- the patient lying face up with feet higher than the head
- the patient lying face down with feet higher than the head
- the patient lying first on one side, then the other, with feet higher than the head
Critical care patients and those depending on mechanical ventilation receive postural drainage therapy four to six times daily. Patients at home are given schedules set by their doctor or respiratory therapist. Percussion and vibration may be performed in conjunction with postural drainage.
Percussion
Percussion, also called cupping or clapping, involves rhythmically striking the chest wall with cupped hands. Mechanical devices can also be used. Percussion results in breaking up thick secretions in the lungs so that they can be more easily removed. Percussion is performed on each lung segment for one to two minutes at a time.
Vibration
Vibration therapy is done for one minute after percussion therapy or may be used instead of percussion therapy for patients who may be too sore or frail to tolerate percussion. The purpose is also to help break up lung secretions. Vibration can be performed either mechanically or manually. When done manually, the person performing the vibration places his or her hands against the patient’s chest and creates vibrations by quickly contracting and relaxing arm and shoulder muscles while the patient exhales. The procedure is repeated several times each day for about five exhalations.
Preparation
Preparation for chest physical therapy starts with an evaluation of the patient’s condition to determine which chest physical therapy techniques would be most beneficial. Since most therapies are done at home, patient education is extremely important. The doctor, nurse, physical therapist, or respiratory therapist instructs the patient or caregiver in chest physical therapy techniques. The therapy should be explained and demonstrated by the health professional. Then the patient or caregiver should try the therapy. This will demonstrate whether the patient understands the therapy or if more instruction is needed.
Aftercare
Patients should be advised to practice oral hygiene procedures to lessen the bad taste and odor of the secretions that they spit out.
Complications
Risks and complications associated with chest physical therapy depend on the health of the patient. Although chest physical therapy usually poses few problems, the health care team should be aware that in some patients it may cause:oxygen deficiency if the head is kept lowered for drainage
- increased intracranial pressure
- temporary low blood pressure
- bleeding in the lungs
- pain or injury to the ribs, muscles, or spine
- vomiting
- inhaling secretions into the lungs
- heart irregularities
Results
The health care team should tell patients that CPT is often an ongoing treatment, with some or all therapies done daily. A positive response to treatment can be assessed by:
- increased volume of sputum secretions
- ease in breathing
- changes in breath sounds
- improved vital signs
- improved chest x ray
- increased oxygen in the blood as measured by arterial blood gas values
Health care team roles
The doctor typically orders chest physical therapy for a patient. A nurse or respiratory therapist provides therapy when a patient is hospitalized. For people seen on an outpatient basis, the emphasis is generally on patient education.
Patient education
Effective patient education is vital because chest physical therapy is often performed at home. A doctor, nurse, or respiratory therapist explains and demonstrates techniques such as breathing, percussion, and incentive spirometry. The patient or caregiver performs the therapy under the health professional’s observation to be sure it can be done correctly independently.
Nurses and respiratory therapists also participate in public awareness education, such as anti-smoking campaigns.
Training
Chest physical therapy is part of training for physicians and nurses specializing in cardiopulmonary treatment, and for respiratory therapists (also known as respiratory care practitioners). Therapists must have at least an associate degree, which is earned after completion of a two-year program. There are also four-year bachelor degree programs for this profession. Graduates with both types of degrees are certified after passing the examination given by the National Board for Respiratory Care.
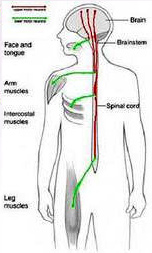
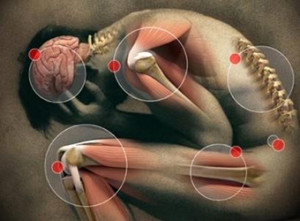
 the brain, spinal cord and all the peripheral nerves to the face, body, arms and legs. Where there is damage to part of the nervous system, whatever the cause be it disease, surgery or accident a specialist physiotherapist working within the field of neurology can help.
the brain, spinal cord and all the peripheral nerves to the face, body, arms and legs. Where there is damage to part of the nervous system, whatever the cause be it disease, surgery or accident a specialist physiotherapist working within the field of neurology can help.









 but your
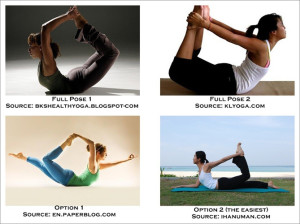
but your baby will love it! You can begin your postnatal exercise and yoga routine after your six-week postnatal check. But remember it is always important to listen to your body and not to push yourself in these early days.
baby will love it! You can begin your postnatal exercise and yoga routine after your six-week postnatal check. But remember it is always important to listen to your body and not to push yourself in these early days. A patient with cystic fibrosis receives chest physical therapy after using nebulizer therapy to loosen the mucus in her lungs.
A patient with cystic fibrosis receives chest physical therapy after using nebulizer therapy to loosen the mucus in her lungs.

 ctions Localized inflammation As in
ctions Localized inflammation As in


 ecoming popular in the West. In fact, many companies, especially in Britain, are seeing the benefit of yoga, recognizing that relaxed workers are healthier and more creative, and are sponsoring yoga fitness programs.
ecoming popular in the West. In fact, many companies, especially in Britain, are seeing the benefit of yoga, recognizing that relaxed workers are healthier and more creative, and are sponsoring yoga fitness programs.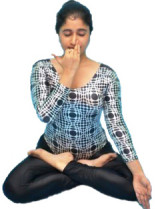

 Often after fracture, the bone needs to be stabilized or immobilized to ensure proper healing. This is usually accomplished using a cast. For simple fractures, your doctor may elect to apply a removable cast so that gentle motion can occur around the injury site. After complex fractures or an ORIF procedure, you may be required to wear a cast that is not to be removed. If you fracture your shoulder or arm, you may be required to wear a sling to keep the arm immobilized. Check with your doctor to ensure that you understand what is expected of you in regard to immobilization.
Often after fracture, the bone needs to be stabilized or immobilized to ensure proper healing. This is usually accomplished using a cast. For simple fractures, your doctor may elect to apply a removable cast so that gentle motion can occur around the injury site. After complex fractures or an ORIF procedure, you may be required to wear a cast that is not to be removed. If you fracture your shoulder or arm, you may be required to wear a sling to keep the arm immobilized. Check with your doctor to ensure that you understand what is expected of you in regard to immobilization.